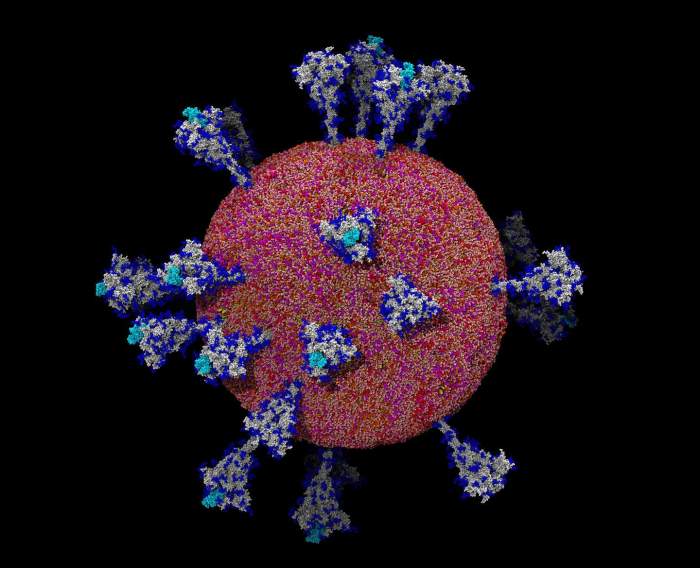
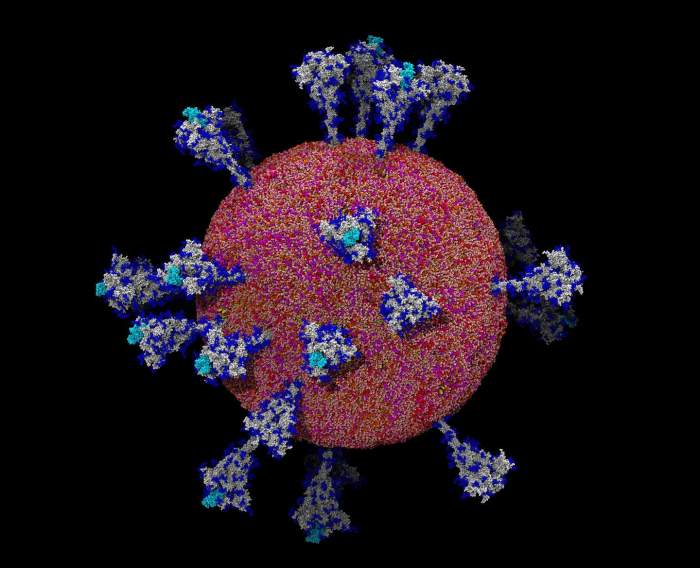
Coronavirus public health emergency sets the stage for this enthralling narrative, offering readers a glimpse into a global crisis that reshaped healthcare systems, daily life, and international collaborations. From the initial surge to the long-term implications, this exploration delves into the defining characteristics of a public health emergency, its impact on healthcare and society, and the global response.
This comprehensive overview examines the defining characteristics of a public health emergency, focusing specifically on the coronavirus pandemic. It analyzes the various facets of this crisis, including the strain on healthcare resources, societal disruptions, and the global response efforts. The historical context of public health emergencies is examined, along with a comparison to other significant events. The narrative culminates in a discussion of long-term implications and lessons learned.
Defining the Public Health Emergency: Coronavirus Public Health Emergency
A public health emergency is a significant disruption to the health of a population, often exceeding the capacity of routine healthcare systems to manage. These events require immediate and coordinated action to prevent further spread and protect public health. The COVID-19 pandemic, with its rapid global spread and substantial impact on healthcare systems, stands as a powerful example of a public health emergency.Understanding the criteria for declaring such an emergency is crucial for effective response and resource allocation.
Defining a public health emergency involves assessing the severity of the threat, the potential for widespread impact, and the need for extraordinary measures. This process, when properly executed, allows for timely and appropriate interventions to mitigate the impact on public health.
With the coronavirus public health emergency still a factor, it’s interesting to see how travel is adapting. JetBlue’s new flight from NYC to Dublin, a route I’ve been wanting to take for ages, is a great example of how things are slowly returning to a more normal state, jetblue new flight nyc dublin. However, the pandemic’s impact on global health remains a significant concern, and responsible travel habits are still crucial.
Criteria for Public Health Emergencies
Public health emergencies are characterized by specific criteria. These criteria, in the context of a pandemic, typically involve a significant increase in cases, a rapid rate of transmission, and the potential for overwhelming healthcare resources. The COVID-19 pandemic demonstrated the crucial need for a prompt and coordinated response to contain the spread.
Historical Context of Public Health Emergencies
The concept of public health emergencies is not new. Throughout history, outbreaks of infectious diseases, like the 1918 influenza pandemic or the 2003 SARS outbreak, have underscored the importance of swift and coordinated responses. These past events highlighted the need for international cooperation, robust surveillance systems, and effective communication strategies. Each instance highlighted specific challenges and lessons learned that shaped subsequent responses to public health emergencies.
The coronavirus public health emergency definitely threw a wrench into travel plans. Luckily, though, options like an overnight train between Prague and Croatia are still a viable way to explore Europe. For those looking to experience the continent, a journey via overnight train between prague croatia is a great way to connect with the region while still maintaining a safe travel strategy during this time.
While we still need to be mindful of safety guidelines, travel can still be an amazing experience, just with a little more consideration.
Roles of International and National Organizations
Multiple organizations play crucial roles in the declaration and response to public health emergencies. The World Health Organization (WHO) serves as the global coordinating body, issuing warnings and guidelines. National governments are responsible for implementing these guidelines within their borders, often establishing emergency response teams and coordinating with local authorities. Other organizations, like the Centers for Disease Control and Prevention (CDC) in the US, provide critical support at the national level.
The collaborative efforts of these organizations are paramount in managing a global public health emergency.
Comparison with Other Significant Public Health Emergencies
Comparing the COVID-19 pandemic with other significant public health emergencies reveals both similarities and differences. The scale and speed of COVID-19’s spread were unprecedented, requiring a global response unlike previous events. However, shared characteristics included the need for robust surveillance, isolation protocols, and resource allocation. The SARS outbreak, while smaller in scope, presented similar challenges in terms of rapid transmission and the need for international collaboration.
Comparing these events highlights the evolving nature of public health emergencies and the importance of adapting response strategies to new challenges.
Navigating the lingering effects of the coronavirus public health emergency can feel overwhelming. Luckily, preparing for potential future travel adventures doesn’t have to be a headache. Check out this handy Amazon winter packing list, curated by travel writers, for a head start on your next trip amazon winter packing list travel writer picks. Whether you’re headed to the slopes or just need cozy winter essentials, these items can make a difference, potentially reducing the anxieties of a future travel scenario, reminding us that life, even during a public health emergency, finds a way to continue.
Key Indicators of Severity and Duration
Determining the severity and duration of a public health emergency, like COVID-19, relies on several key indicators. These indicators include the number of confirmed cases and deaths, the rate of transmission, the capacity of healthcare systems to handle the influx of patients, and the availability of effective treatments and vaccines. The availability of effective treatments and vaccines is critical to limiting the severity and duration of the emergency.
Monitoring these indicators is vital for adjusting interventions and anticipating future needs. For example, the initial rapid increase in COVID-19 cases in various regions led to lockdowns and social distancing measures to mitigate the spread. The gradual decline in cases after vaccination programs demonstrated the impact of these strategies.
Impact on Healthcare Systems
The coronavirus pandemic exerted unprecedented pressure on healthcare systems globally. The immediate and long-term consequences were far-reaching, affecting resource allocation, staffing levels, and the very fabric of medical care. This crisis exposed vulnerabilities and forced a re-evaluation of healthcare infrastructure and preparedness.
Immediate Impacts on Healthcare Resources
The surge in COVID-19 cases overwhelmed healthcare systems worldwide. Hospitals faced a critical shortage of beds, intensive care unit (ICU) beds, and ventilators. The need for surge capacity was acutely felt in many regions, as hospitals struggled to accommodate the influx of patients. Staffing became a significant issue, with healthcare workers facing burnout and high infection rates.
The rapid spread of the virus necessitated the implementation of stringent infection control measures, further impacting operational efficiency.
Long-Term Impacts on Healthcare Systems
The long-term impacts extended beyond the immediate crisis. The pandemic accelerated the digital transformation of healthcare, with telehealth and remote monitoring becoming more prevalent. However, equitable access to these technologies remained a challenge, highlighting existing disparities in healthcare access. The crisis underscored the importance of robust pandemic preparedness plans, including strategies for surge capacity, supply chain management, and workforce development.
Hospitals experienced increased financial strain, impacting their ability to invest in research and future infrastructure.
Strain on Healthcare Resources
The strain on healthcare resources was multifaceted. Hospitals struggled to maintain adequate supplies of personal protective equipment (PPE), testing kits, and medications. The demand for healthcare professionals exceeded the supply, leading to burnout and staff shortages. The strain was particularly acute in regions with limited healthcare infrastructure. This underscored the critical need for investment in healthcare infrastructure, particularly in developing countries.
Impact on Research and Development
The pandemic spurred unprecedented research and development efforts to combat the virus. This included the rapid development of vaccines and treatments, demonstrating the potential for accelerated scientific progress in response to a global crisis. However, the long-term implications for research and development in other areas of healthcare were uncertain. The diversion of resources to COVID-19 research may have delayed progress in other areas.
Financial Implications
The financial implications for healthcare institutions and governments were substantial. Hospitals incurred significant costs associated with increased patient care, infection control measures, and staff compensation. Governments faced substantial expenditures for public health initiatives, testing, and treatment. The financial burden placed a strain on healthcare systems worldwide, raising concerns about the sustainability of healthcare provision.
Variations in Healthcare System Responses
| Country | Initial Response | Long-Term Impact | Lessons Learned |
|---|---|---|---|
| United States | Initially slow and inconsistent response, with significant disparities in access to care across states. | Increased financial strain on hospitals, exacerbated existing healthcare inequalities. | Need for a more unified and coordinated national response to future crises. |
| South Korea | Rapid, effective contact tracing and testing strategies, along with aggressive public health measures. | Demonstrated the importance of proactive public health measures in mitigating the spread of the virus. | Early and effective response strategies can significantly limit the spread of the virus and its impact. |
| United Kingdom | Initially focused on protecting the NHS, but faced challenges in managing the surge in cases. | Significant strain on the NHS, leading to long-term impacts on patient care. | Importance of robust surge capacity planning and proactive measures for mitigating the spread of the virus. |
| India | Faced a tremendous challenge due to the sheer volume of cases and limited resources. | Significant loss of life, and a strain on healthcare infrastructure. | Need for increased investment in healthcare infrastructure and surge capacity. |
Societal Impacts

The coronavirus pandemic profoundly reshaped societal structures and daily routines. From economic downturns to profound mental health crises, the impacts were far-reaching and varied across demographics. The crisis exposed vulnerabilities in existing systems and prompted unprecedented responses from communities and governments alike.
Economic Disruptions
The pandemic triggered a global economic downturn, with businesses closing, industries shrinking, and unemployment rates soaring. Supply chains were disrupted, impacting international trade and domestic markets. Lockdowns and social distancing measures significantly hampered economic activity, leading to widespread job losses and financial hardship. Small businesses, particularly in the service sector, were disproportionately affected. The pandemic highlighted the interconnectedness of the global economy and the fragility of economic systems in the face of a widespread health crisis.
Social Distancing Measures, Coronavirus public health emergency
Social distancing measures, including lockdowns and restrictions on public gatherings, were implemented globally to curb the spread of the virus. These measures drastically altered daily life, forcing people to adapt to new ways of working, learning, and socializing. Remote work became the norm for many, while schools transitioned to online learning. Social interactions were limited to virtual platforms, leading to a decline in social contact and a sense of isolation for many individuals.
Communities found innovative ways to maintain social connections, fostering online communities and supporting each other through virtual events and initiatives.
Mental Health Concerns
The pandemic exerted immense pressure on mental well-being. The uncertainty, isolation, and fear associated with the virus contributed to increased rates of anxiety, depression, and stress. Healthcare systems were overwhelmed, leading to delays in mental health care and support. The disruption to daily routines, job losses, and the constant threat of infection created significant psychological distress, especially among vulnerable populations.
The crisis underscored the importance of mental health support and resources in times of crisis.
Changes in Daily Life and Routines
Daily life was dramatically transformed by the pandemic. Working from home became commonplace, altering commuting patterns and office environments. Social interactions shifted from in-person gatherings to virtual platforms. Education moved online, changing the learning experience for students. These changes had profound impacts on individuals’ routines, social lives, and work-life balance.
People adapted to new routines, often juggling multiple roles and responsibilities while maintaining social distancing measures.
Community Adaptations
Communities responded creatively and collaboratively to the public health emergency. Neighborhood support networks emerged, providing essential resources and mutual aid. Local businesses adapted by offering delivery services and pivoting to meet changing demands. Volunteers stepped forward to assist vulnerable populations, providing food, supplies, and emotional support. These community-driven initiatives highlighted the resilience and adaptability of human beings in times of crisis.
Impact on Vulnerable Populations
Vulnerable populations, including the elderly, low-income individuals, and people with pre-existing health conditions, were disproportionately affected by the pandemic. Limited access to healthcare, economic instability, and social isolation exacerbated existing inequalities. The crisis exposed systemic inequalities and highlighted the need for targeted interventions to protect and support vulnerable groups.
Table: Societal Sector Responses
| Sector | Immediate Response | Long-Term Adjustments | Challenges Faced |
|---|---|---|---|
| Education | Transition to online learning, reduced class sizes, increased hygiene measures | Development of hybrid learning models, increased focus on digital literacy, infrastructure improvements | Digital divide, access to technology, maintaining student engagement |
| Healthcare | Increased capacity, prioritizing critical care, implementing infection control protocols | Improved telehealth access, strengthening public health infrastructure, developing new treatments and vaccines | Staff shortages, supply chain disruptions, maintaining patient trust |
| Economy | Government stimulus packages, business closures, job losses | Increased automation, remote work adoption, diversification of supply chains | Economic recession, inflation, business closures, unemployment |
| Transportation | Reduced public transport use, increased car usage, travel restrictions | Investment in public transportation upgrades, promoting sustainable transportation options, re-evaluating urban planning | Reduced revenue for transportation providers, increased congestion, potential for environmental impact |
Global Response and Collaboration
The COVID-19 pandemic underscored the interconnectedness of the world and the crucial need for global cooperation in public health emergencies. Countries, organizations, and individuals faced a shared challenge, demanding a coordinated global response to contain the virus’s spread and mitigate its impact. The response involved a complex interplay of scientific advancements, logistical challenges, and political considerations.The international community’s response was multifaceted, encompassing research, resource allocation, communication, and collaboration among nations.
Different nations had varying levels of preparedness and resources, highlighting the necessity for global support and equitable distribution of aid. This global collaboration was essential to mitigate the pandemic’s devastating effects and facilitate a swift recovery.
International Organizations’ Role
The World Health Organization (WHO) played a pivotal role in coordinating the global response. The WHO acted as a central hub for information dissemination, guiding principles, and technical support. Their efforts included issuing guidelines, providing technical expertise, and mobilizing resources to assist countries in their response. The WHO’s role was crucial in establishing global standards for diagnosis, treatment, and prevention, promoting a coordinated approach across the globe.
Furthermore, their efforts to combat misinformation and promote evidence-based strategies were critical in the face of the pandemic’s uncertainty.
Effectiveness of International Collaborations
The effectiveness of international collaborations varied across different aspects of the pandemic response. While some collaborations yielded significant results in areas like vaccine development and research, others faced challenges related to resource allocation and communication. For instance, the rapid development of several COVID-19 vaccines demonstrated the effectiveness of international collaboration in scientific research. However, unequal access to vaccines in different regions highlighted disparities in resource distribution, underscoring the need for more equitable global health initiatives.
Communication Strategies
Effective communication was vital to the global response. Clear and consistent communication strategies, developed and disseminated by international organizations and national governments, were essential to inform the public about the virus, its transmission, prevention measures, and treatment options. Different countries employed various communication channels, from public service announcements to social media campaigns, to reach their populations effectively. The ability to disseminate timely and accurate information played a critical role in managing public anxieties and promoting adherence to preventive measures.
Sharing of Scientific Data and Research Findings
The rapid exchange of scientific data and research findings was critical in understanding the virus and developing effective interventions. International collaborations facilitated the sharing of information on viral characteristics, transmission dynamics, diagnostic methods, and treatment options. The development of rapid diagnostic tests and effective treatments depended heavily on the timely and transparent exchange of scientific knowledge. Platforms for sharing research, such as preprint servers and scientific journals, played a significant role in accelerating the pace of discovery and knowledge dissemination.
This collaboration was essential in accelerating the development of effective interventions.
Public Health Measures and Policies
The COVID-19 pandemic necessitated a global response, prompting various public health measures and policies aimed at controlling the virus’s spread. These interventions, while crucial, presented complex challenges and trade-offs between public health and societal well-being. Understanding the effectiveness and limitations of these strategies is essential for future pandemic preparedness.
Public Health Interventions Implemented
Numerous public health interventions were implemented worldwide to curb the spread of the virus. These included social distancing measures, lockdowns, mask mandates, contact tracing, quarantine protocols, and vaccination campaigns. The severity and duration of these measures varied considerably across different countries, often reflecting their unique epidemiological situations and political contexts.
Effectiveness and Limitations of Public Health Interventions
The effectiveness of various public health interventions varied depending on factors such as the specific implementation strategy, community compliance, and the virus’s transmissibility. Social distancing and lockdowns, while proven effective in reducing transmission rates, also resulted in significant economic disruptions and mental health challenges. Mask mandates, while showing promising results in controlled environments, faced challenges in public acceptance and adherence.
Contact tracing, when combined with effective isolation and quarantine measures, proved valuable in identifying and interrupting transmission chains, but its effectiveness was often hampered by resource constraints and logistical complexities. Vaccination campaigns, considered a crucial tool in mitigating the pandemic’s impact, were highly successful in reducing severe illness and death, but faced challenges in vaccine hesitancy and equitable distribution.
Examples of Successful and Unsuccessful Public Health Strategies
Successful public health strategies included the swift implementation of widespread vaccination programs in some countries, which dramatically reduced hospitalizations and deaths. Effective contact tracing and quarantine measures in certain regions helped to contain outbreaks and prevent further transmission. Conversely, inconsistent or poorly implemented measures in some areas led to prolonged outbreaks and higher death tolls. The varied levels of public compliance with guidelines also influenced the success of implemented measures.
Comparative Analysis of Public Health Policies Across Countries
Different countries adopted distinct public health policies in response to the pandemic. This divergence stemmed from varying levels of healthcare infrastructure, economic conditions, political systems, and public trust in government. Comparing these policies offers valuable insights into the effectiveness of different approaches.
Table: Comparative Analysis of Public Health Policies
| Country | Policy 1 (e.g., Lockdowns) | Policy 2 (e.g., Mask Mandates) | Outcome (e.g., Cases, Deaths) |
|---|---|---|---|
| United States | Varied, often localized and inconsistent | Initially resisted, later adopted inconsistently | High case and death counts |
| South Korea | Early and aggressive lockdowns and contact tracing | Widespread mask usage | Lower case and death counts compared to US |
| Singapore | Strict lockdowns and border controls | Mandatory mask usage and high compliance | Low case and death counts |
| New Zealand | “Zero-Covid” approach with strict lockdowns and border controls | Mandatory mask usage and high compliance | Very low case and death counts |
Long-Term Implications and Lessons Learned
The COVID-19 pandemic, a global public health emergency, profoundly reshaped healthcare systems, economies, and societies. Beyond the immediate crisis, lasting implications emerged across various sectors, prompting critical reflection on preparedness and response mechanisms. The pandemic highlighted both strengths and weaknesses in existing systems, paving the way for necessary adjustments and improvements.The pandemic forced a rapid adaptation to remote work, virtual learning, and telehealth, altering daily routines and work patterns.
This shift underscored the need for more resilient and adaptable systems, particularly in the face of future crises. The experiences gained during the emergency serve as a valuable resource for future public health crises.
Long-Term Impacts on Healthcare Systems
The pandemic accelerated the adoption of telehealth, remote monitoring, and digital health tools. These innovations, while initially implemented as temporary solutions, demonstrated their potential for improving access to care, particularly for underserved populations and those in remote areas. Furthermore, the pandemic highlighted the critical need for robust supply chains for essential medical supplies and equipment. The global shortage of personal protective equipment (PPE) during the initial stages of the pandemic underscored the need for better forecasting and stockpiling mechanisms.
Hospitals and healthcare facilities also had to adapt to surge capacity demands, requiring better planning for future events.
Societal Impacts and Policy Changes
The pandemic significantly impacted various aspects of daily life, including social interactions, education, and economic activity. The rapid spread of misinformation and disinformation highlighted the need for robust communication strategies and reliable information sources during public health emergencies. Moreover, the pandemic spurred policy changes regarding public health preparedness and response. Countries and organizations began prioritizing investments in public health infrastructure, research, and surveillance systems.
These changes demonstrate the critical importance of proactive measures in mitigating future public health crises.
Lessons Learned About Public Health Preparedness
The pandemic revealed critical gaps in public health preparedness and response. The global response to the pandemic exposed significant disparities in healthcare access and resource allocation across different regions and populations. A lack of international collaboration and coordinated action hindered the global response in the initial stages. This underscored the need for enhanced global cooperation and coordination in future crises.
- Enhanced Surveillance Systems: The pandemic underscored the importance of robust and real-time surveillance systems to detect and respond to emerging infectious diseases. Early detection and rapid response are crucial for containing outbreaks and preventing widespread transmission. This necessitates strengthening epidemiological surveillance networks and enhancing data sharing protocols.
- Improved Communication Strategies: Effective communication is essential for maintaining public trust and compliance with public health measures. Clear, concise, and consistent messaging from credible sources can significantly impact public behavior during a crisis. Misinformation and disinformation campaigns can be countered by proactive and well-targeted communication strategies.
- Strengthened Global Collaboration: International collaboration and coordination are essential for a unified global response to public health emergencies. Sharing best practices, resources, and expertise across borders can accelerate the development and implementation of effective interventions.
Examples of Improved Public Health Systems
The pandemic spurred innovations in public health systems, leading to more efficient and effective practices. The rapid development and deployment of vaccines highlight the importance of robust research and development capabilities. The accelerated development of diagnostic tools and treatments demonstrate the potential for rapid scientific advancements.
- Digital Health Tools: Telehealth platforms and remote monitoring technologies have become more widely adopted, improving access to care for vulnerable populations and enhancing the efficiency of healthcare delivery. This trend is expected to continue and further expand.
- Public Health Infrastructure: Investments in public health infrastructure, such as laboratories, surveillance systems, and contact tracing teams, have been prioritized to better prepare for future outbreaks. This demonstrates a long-term commitment to strengthening public health systems.
Preparedness for Future Public Health Emergencies
Learning from the COVID-19 pandemic, future preparedness strategies must focus on strengthening global cooperation, enhancing surveillance systems, and improving communication strategies. Proactive measures are necessary to mitigate the impacts of future public health crises. Investing in public health infrastructure and research and development capabilities will ensure a faster and more coordinated response to future emergencies.
Epilogue
The coronavirus public health emergency was a defining moment in recent history, impacting every facet of global life. The lessons learned from this crisis are crucial for future preparedness and response. This analysis highlights the interconnectedness of global health and the importance of international collaboration, while also emphasizing the need for robust healthcare systems and adaptive societal measures to navigate future public health crises.
The long-term implications of the pandemic extend beyond immediate recovery, shaping future policies and practices.

Leave a Reply